by admin | Aug 7, 2017 | ACA, Employee Benefits, Health & Wellness
Preexisting conditions. While it’s no doubt this term has been a hot topic in recent months—and notably misconstrued—one thing has not changed; insurers cannot deny coverage to anyone with a preexisting condition. Now that House Resolution 1628 has moved to the Senate floor, what can employers and individuals alike expect? If passed by the Senate as is and signed into law; some provisions will take place as early as 2019—possibly 2018 for special enrollment cases. It’s instrumental for companies to gear up now with a plan on how to tackle open enrollment; regardless of whether your company offers medical coverage or not.
Under the current proposed American Health Care Act (AHCA) insurance companies can:
- Price premiums based on health care status/age. The AHCA will provide “continuous coverage” protections to guarantee those insured are not charged more than the standard rate as long as they do not have a break in coverage. However, insurers will be allowed to underwrite certain policies for those that do lapse—hence charging up to 30% more for a preexisting condition if coverage lapses for more than 63 days. This is more common than not, especially for those who are on a leave of absence for illness or need extensive treatment. In addition, under current law, insurers are only allowed to charge individuals 50 and older 3 times as much than those under this age threshold. This ratio will increase 5:1 under AHCA.
- Under the ACA’s current law employers must provide coverage for 10 essential health care benefits. Under AHCA, beginning as early as 2020, insurers will allow states to mandate what they consider essential benefit requirements. This could limit coverage offered to individuals and within group plans by eliminating high cost care like mental health and substance abuse. Not that it’s likely, but large employers could eventually opt out whether they want to provide insurance and/or choose the types of coverage they will provide to their employees.
It’s important to note that states must apply for waivers to increase the ratio on insurance premiums due to age, and determine what they will cover for essential health benefits. In order to have these waivers granted, they would need to provide extensive details on how doing so will help their state and the marketplace.
So what can employers do moving forward? It’s not too soon to think about changing up your benefits package as open enrollment approaches, and educating yourself and your staff on AHCA and what resources are out there if you don’t offer health coverage.
- Make a variety of supplemental tools available to your employees. Anticipate the coming changes by offering or adding more supplemental insurance and tools to your benefits package come open enrollment. Voluntary worksite benefits, such as Cancer, Critical Illness, and Accident Insurance handle a variety of services at no out-of-pocket cost to the employer. HSA’s FSA’s and HRA’s are also valuable supplemental tools to provide your employees if you’re able to do so. Along with the changes listed above, the AHCA has proposed to also increase the contribution amounts in these plans and will allow these plans to cover Over-the-Counter (OTC) medications.
- Continue to customize wellness programs. Most companies offer wellness programs for their employees. Employers that provide this option should continue advancing in this area. Addressing the specific needs of your employees and providing wellness through various platforms will result in the greatest return on investment; and healthier employees to boot. Couple this with frequent evaluations from your staff on your current program to determine effectiveness and keep your wellness programs on point.
- Educate, educate, educate—through technology. Regardless if you employ 10 or 10,000, understanding benefit options is vital for your employees; what you have to offer them and what they may need to know on their own. Digital platforms allow individuals to manage their healthcare benefits and stay in the know with valuable resources at their fingertips. There’s no limit on the mediums available to educate your employees on upcoming changes. Partnering with a strong benefit agency to maximize these resources and keep your employees “in the know” during a constantly changing insurance market is a great way to start.

by admin | Aug 4, 2017 | HSA/HRA
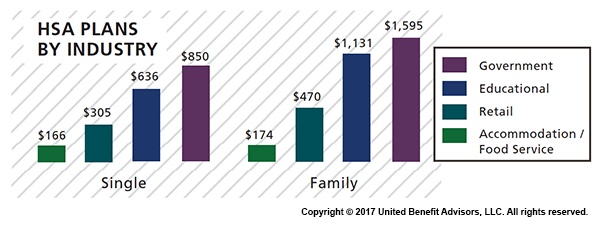
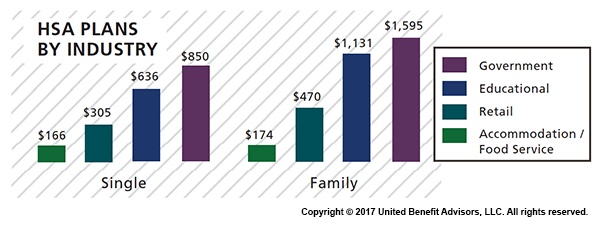
 Across most industries, HSA contributions are, for the most part, down or unchanged from three years ago, according to UBA’s Health Plan Survey. The average employer contribution to an HSA is $474 for a single employee (down 3.5 percent from 2015 and 17.6 percent from five years ago) and $801 for a family (down 9.2 percent from last year and 13.7 percent from five years ago). Government and education employers are the only industries with average single contributions well above average and on the rise.
Across most industries, HSA contributions are, for the most part, down or unchanged from three years ago, according to UBA’s Health Plan Survey. The average employer contribution to an HSA is $474 for a single employee (down 3.5 percent from 2015 and 17.6 percent from five years ago) and $801 for a family (down 9.2 percent from last year and 13.7 percent from five years ago). Government and education employers are the only industries with average single contributions well above average and on the rise.
Government employees had the most generous contributions for singles at $850, on average, up from $834 in 2015. This industry also has the highest employer contributions for families, on average, at $1,595 (though that is down from 1,636 in 2015). Educational employers are the next most generous, contributing $636, on average, for singles and $1,131 for families.
Singles in the accommodation/food services industries received virtually no support from employers, with average HSA contributions at $166. The same is true for families with HSA plans in the accommodation/food services industries with average family contributions of $174.
Retail employers also remain among the least generous contributors to single and family HSA plans, contributing $305 and $470, respectively. This may be why they have low enrollment in these plans.
The education services industry has seen a 109 percent increase in HSA enrollment since 2013 (aided by employers’ generous contributions), catapulting the industry to the lead in HSA enrollment at 23.8 percent. The professional/scientific/tech and finance/insurance industries follow closely at 23.3 percent and 22.1 percent, respectively.
The mining/oil/gas industry sees the lowest enrollment at 3.8 percent. The retail, hotel, and food industries continue to have some of the lowest enrollment rates despite the prevalence of these plans, indicating that these industries, in particular, may want to increase employee education efforts about these plans and how they work.
For a detailed look at the prevalence and enrollment rates among HSA and HRA plans by group size and region, view UBA’s “Special Report: How Health Savings Accounts Measure Up”.
Benchmarking your health plan with peers of a similar size, industry or geography makes a big difference in determining if your plan is competitive. To compare your exact plan with your peers, request a custom benchmarking report.
For fast facts about HSA and HRA plans, including the best and worst plans, average contributions made by employers, and industry trends, download (no form!) “Fast Facts: HSAs vs. HRAs”.
By Bill Olson
Originally Posted By www.ubabenefits.com

by admin | Jul 31, 2017 | COBRA, Human Resources
 The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires group health plans to provide notices to covered employees and their families explaining their COBRA rights when certain events occur. The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan. This notice is issued by the plan administrator within the first 90 days when coverage begins under the group health plan and informs the covered employee (and his or her spouse) of the responsibility to notify the employer within 60 days if certain qualifying events occur in the future.
The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires group health plans to provide notices to covered employees and their families explaining their COBRA rights when certain events occur. The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan. This notice is issued by the plan administrator within the first 90 days when coverage begins under the group health plan and informs the covered employee (and his or her spouse) of the responsibility to notify the employer within 60 days if certain qualifying events occur in the future.
The initial notice must include the following information:
- The plan administrator’s contact information
- A general description of the continuation coverage under the plan
- An explanation of the covered employee’s notice obligations, including notice of
- The qualifying events of divorce, legal separation, or a dependent’s ceasing to be a dependent
- The occurrence of a second qualifying event
- A qualified beneficiary’s disability (or cessation of disability) for purposes of the disability extension)
- How to notify the plan administrator about a qualifying event
- A statement that the notice does not fully describe continuation coverage or other rights under the plan, and that more complete information regarding such rights is available from the plan administrator and in the plan’s summary plan description (SPD)
As a best practice, the initial notice should also:
- Direct qualified beneficiaries to the plan’s most recent SPD for current information regarding the plan administrator’s contact information.
- For plans that include health flexible spending arrangements (FSAs), disclose the limited nature of the health FSA’s COBRA obligations (because certain health FSAs are only obligated to offer COBRA through the end of the year to qualified beneficiaries who have underspent accounts).
- Explain that the spouse may notify the plan administrator within 60 days after the entry of divorce or legal separation (even if an employee reduced or eliminated the spouse’s coverage in anticipation of the divorce or legal separation) to elect up to 36 months of COBRA coverage from the date of the divorce or legal separation.
- Define qualified beneficiary to include a child born to or placed for adoption with the covered employee during a period of COBRA continuation coverage.
- Describe that a covered child enrolled in the plan pursuant to a qualified medical child support order during the employee’s employment is entitled to the same COBRA rights as if the child were the employee’s dependent child.
- Clarify the consequences of failing to submit a timely qualifying event notice, timely second qualifying event notice, or timely disability determination notice.
Practically speaking, the initial notice requirement can be satisfied by including the general notice in the group health plan’s SPD and then issuing the SPD to the employee and his or her spouse within 90 days of their group health plan coverage start date.
If the plan doesn’t rely on the SPD for furnishing the initial COBRA notice, then the plan administrator would follow the U.S. Department of Labor (DOL) rules for delivery of ERISA-required items. A single notice addressed to the covered employee and his or her spouse is allowed if the spouse lives at the same address as the covered employee and coverage for both the covered employee and spouse started at the time that notice was provided. The plan administrator is not required to provide an initial notice for dependents.
By Danielle Capilla
Originally Posted By www.ubabenefits.com

by admin | Jul 25, 2017 | Group Benefit Plans, Health Plan Benchmarking
 Modern medicines have resulted in longer, more productive lives for many of us. Prescription drugs soothe sore muscles after a strenuous workout or manage the conditions of a chronic disease. Unfortunately, this use of prescriptions drugs can come with a hefty price tag.
Modern medicines have resulted in longer, more productive lives for many of us. Prescription drugs soothe sore muscles after a strenuous workout or manage the conditions of a chronic disease. Unfortunately, this use of prescriptions drugs can come with a hefty price tag.
Americans are spending more money on prescription drugs than ever before and the United States as a nation spends more per capita on prescription drugs than any other country. With the cost of some drugs exceeding thousands of dollars for a 30-day supply, this can translate into financial hardship for many Americans.
For employers sponsoring a medical plan, managing the cost of these prescription drugs is also becoming a task. Insurance companies and employers struggle with the ability to provide affordable medical plans, and the ever-increasing prescription drug costs are a primary driver of this difficulty. As a result, prescription drug plan designs are changing shape – moving to a model that helps push more of the cost of these drugs to the member along with increasing awareness of the true cost of the prescriptions.
Flat dollar copay plans have become an expected norm in medical plans for almost a decade. However, insurance companies underwriting fully insured medical plans and employers sponsoring self-funded medical programs now need to make modifications to these plan designs to manage the ever-increasing prescription drug costs. As a result, we are seeing more prescription drug plans combining some aspect of coinsurance along with or in place of the flat dollar copayments.
According to the 2016 UBA Health Plan Survey, copay models are still the most popular, with a three-tier copay structure the most prevalent. Median retail copayments for these three-tier plans are $10 for generic drugs, $35 for preferred brand drugs (drugs on the carrier’s prescription drug list) and $60 for non-preferred brand drugs (drugs not on the carrier’s prescriptions drug list). While 54.5 percent of all prescription plans are copay only, approximately 40 percent of all prescription drug plans have co-insurance along with (or in lieu of) copays–a plan design that is particularly common among four-tier plans.
Coinsurance models have many unique designs. Some plans are a straight percentage of the cost of the drug; some may involve a maximum or minimum dollar copayment combined with the coinsurance. For example, a plan may require 40 percent coinsurance for a preferred brand drug, but there is a minimum copayment of $30 and a maximum copayment of $50. Typically, we see a higher coinsurance percentage for non-preferred brand drugs and specialty drugs. The member cost of the drug is calculated after any negotiated discounts, so members covered by a coinsurance plan are reaping the benefits of any discounts negotiated with the pharmacy by the pharmacy benefit manager (PBM).
Coinsurance plans do provide several advantages to managing prescription drug costs. Under a flat dollar copay plan design, members may not truly understand the full cost of the drug they are purchasing. Pharmacies are now disclosing the full cost of drugs on the purchase receipts. Yet, most consumers do not take note of this disclosure, focusing only on the copayment amount. When a member pays a percentage of the cost of the drug as in a coinsurance model, the true cost of the drug becomes much more apparent.
Another advantage of the coinsurance model is that it automatically increases the member share of the cost as the price of the drug increases. Under the flat dollar copayment model, as the true cost of the drug increases, the member pays a smaller portion of the total cost. When the member’s portion is determined by a coinsurance percentage, the member pays more as the cost of the drug increases.
As the costs of health care overall continue to increase, we all need to become better consumers of our healthcare. Members covered by a prescription drug plan with a coinsurance model will have a better understanding of the true cost of their prescriptions. As members become more aware of the true costs of their care, they make better health care decisions, managing the overall cost of care.
We expect to see prescription drug benefit plans change even more as the cost of health care – especially prescription drugs – escalates. These changes will likely result in more of the cost being pushed to the patient. There are resources available to patients for assistance with some of these out-of-pocket costs. It is vital for the patient to understand their costs and know how to maximize their benefits. In a few weeks, the UBA blog will highlight some of these resources and provide information on how to educate employees on maximizing their benefits and the industry resources available to them.
For all the cost and design trends related to health and prescription drug plan costs by group size, industry and region, download UBA’s Health Plan Survey Executive Summary.
By Mary Drueke-Collins
Originally Posted By www.ubabenefits.com
by admin | Jul 20, 2017 | Benefit Management, ERISA
UBA’s compliance team leverages the collective expertise of its independent partner firms to advise 36,000 employers and their 5 million employees. Lately, a common question from employers is: If a health and welfare benefit plan has fewer than 100 participants, then does it need to file a Form 5500?
If a plan is self-funded and uses a trust, then it is required to file a Form 5500, no matter how many participants it has.
Whether the plan must file a Form 5500 depends on whether or not the plan is “unfunded” (where the money comes from to pay for the self-funded claims).
Currently, group welfare plans generally must file Form 5500 if:
- The plan is fully insured and had 100 or more participants on the first day of the plan year (dependents are not considered “participants” for this purpose unless they are covered because of a qualified medical child support order).
- The plan is self-funded and it uses a trust, no matter how many participants it has.
- The plan is self-funded and it relies on the Section 125 plan exemption, if it had 100 or more participants on the first day of the plan year.
There are several exemptions to Form 5500 filing. The most notable are:
- Church plans defined under ERISA Section 3(33)
- Governmental plans, including tribal governmental plans
- Top hat plans which are unfunded or insured and benefit only a select group of management or highly compensated employees
- Small insured or unfunded welfare plans. A welfare plan with fewer than 100 participants at the beginning of the plan year is not required to file an annual report if the plan is fully insured, entirely unfunded, or a combination of both.
A plan is considered unfunded if the employer pays the entire cost of the plan from its general accounts. A plan with a trust is considered funded.
For smaller groups that are self-funded or partially self-funded, you’d need to ask them whether the plan is funded or unfunded.
If the employer pays the cost of the plan from general assets, then it is considered unfunded and essentially there is no trust.
If the employer pays the cost of the plan from a specific account (in which plan participant contributions are segregated from general assets), then the plan is considered funded. For example, under ERISA, pre-tax salary reductions under a cafeteria plan are participant contributions and are considered plan assets which must generally be held in trust based on ERISA’s exclusive benefit rule and other fiduciary duty rules.
By Danielle Capilla
Originally Posted By www.ubabenefits.com